Will the Veterans Affairs (VA) pay for a massage chair? It is an important one for veterans seeking relief from various health conditions. Let's check out with a comprehensive overview of the VA's policies and programs related to massage therapy and massage chairs, providing clarity on what benefits may be available to veterans.
VA Coverage for Massage Chairs?
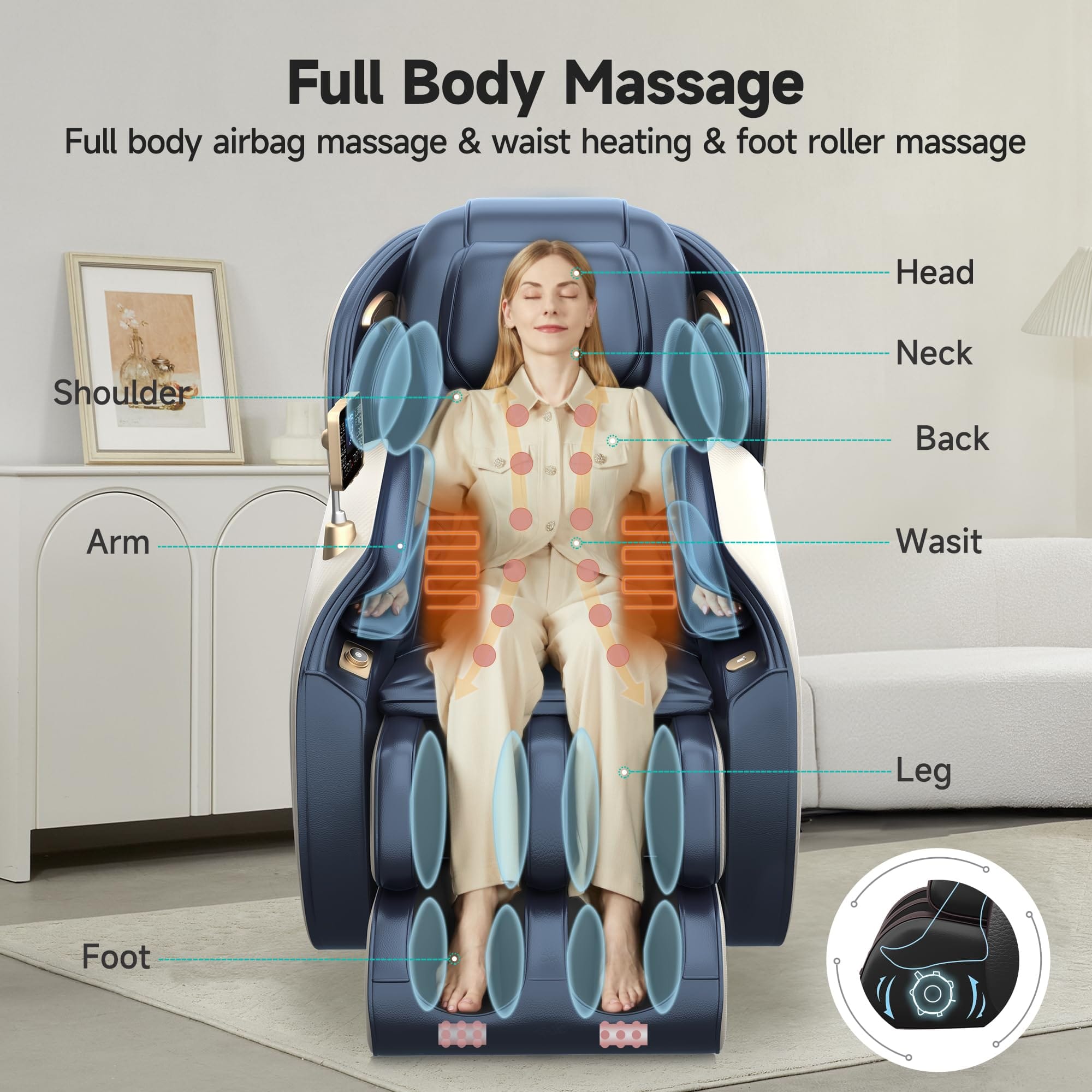
The VA does not typically cover the cost of a massage chair as a standard benefit. Recliner massage chairs are not classified as Durable Medical Equipment (DME) under the VA's coverage policies, which means they are not eligible for direct insurance coverage. The VA's DME program provides free prosthetic appliances, equipment, and services for veterans receiving VA care for any condition, but this list does not include massage chairs.
VA Recognizes Massage Therapy
While the VA does not cover massage chairs, it does recognize the therapeutic benefits of massage therapy for veterans. Massage therapy can be covered by the VA under certain conditions, particularly when it is deemed medically necessary for managing pain, PTSD, and other chronic conditions.
Eligibility and Accessing Massage Therapy Services
Veterans who are enrolled in VA healthcare and have a service-connected disability, receive a VA pension, or have lower income levels are more likely to be eligible for comprehensive health benefits, including complementary and integrative health services like massage therapy. To access these services, veterans should:
Enroll in VA Healthcare
This can be done online, by phone, or in person at a VA medical center.
Schedule a Consultation
Meet with their primary care provider at the VA to discuss the need for massage therapy and how it could help manage specific health issues.
Request a Referral
If the provider agrees that massage therapy would be beneficial, they can issue a referral to a VA medical center that offers these services or authorize care through the VA’s Community Care Program.
VA Community Care Program
If the VA facility does not provide massage therapy services directly, veterans may be able to receive care from a community provider through the VA Community Care Program. This program allows veterans to access healthcare services outside of the VA network under certain conditions, such as geographic inaccessibility or the unavailability of the required service at the nearest VA facility.
Navigating Coverage and Payment
The VA typically covers the cost of massage therapy services if they are deemed medically necessary and provided through an authorized VA or community provider. All services must be pre-authorized by the VA to ensure they will be covered. The massage therapy provider should bill the VA directly for services rendered, and veterans should not be charged out-of-pocket if the service is authorized and provided within the VA network or Community Care Program.
Additional Resources and Support
Veterans who encounter difficulties in accessing massage therapy services or who need assistance navigating the VA system can seek help from VA Patient Advocates, Veterans Service Organizations (VSOs), or VA Complementary and Integrative Health Coordinators.
In summary, while the VA does not directly pay for massage chair recliners, they do offer benefits that can help veterans access massage therapy services, which can provide similar therapeutic benefits. Veterans are encouraged to discuss their needs with their healthcare providers to explore all available options and benefits. Understanding the referral process, eligibility criteria, and available resources is key to successfully obtaining these benefits.






























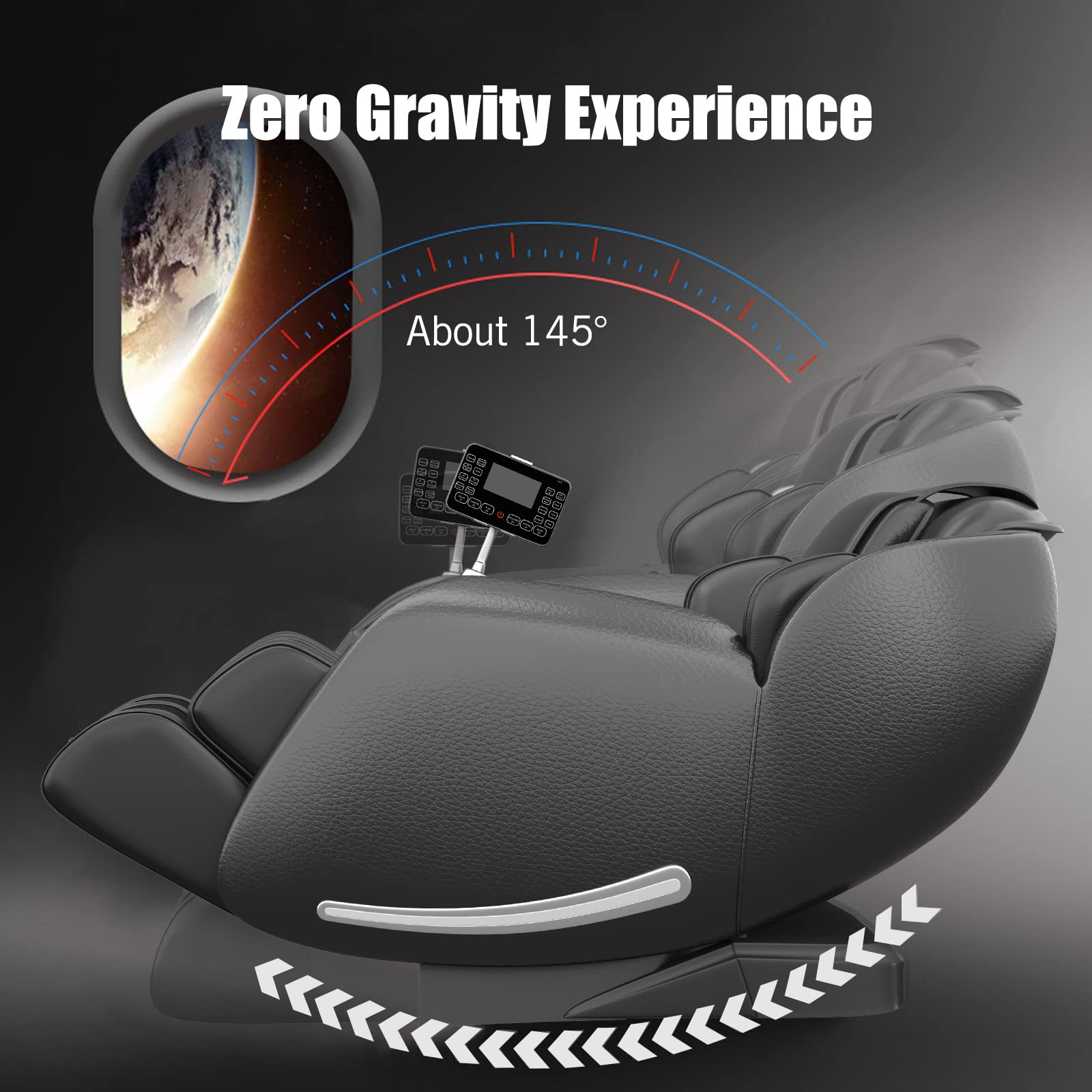












I’m currently receiving Massage therapy 2 days and week for 12 weeks and the cost is 149.00 a session equals 3,576.00. Some chairs or less than 2000.00. If the va pay half the cost I could finance the other half Wayfair has them under 1000.00 this would help me with the pain and anxiety I go through every day, when I finish my sessions a day and / or two later the pain returns I’m back in the state I was before the massage. We could save millions in health care expenses from community care services. We need to put this to The VA president.